Our 3-in-1 approach
94% of patients report pain severity improvement with a cannabis-based medication plan.
1️⃣
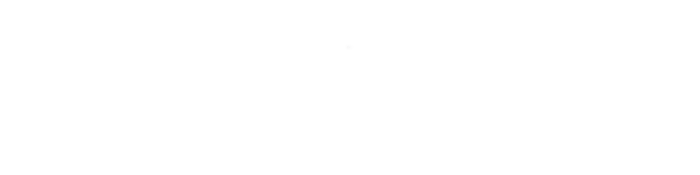
1-1 support from your own team of pain experts
The best of the NHS
Our team are known for their compassionate care for complex conditions, especially those often unrecognised and overlooked.
Between them they’ve run NHS pain clinics, been elected leaders of leading pain institutions and helped write the NICE guidelines on chronic pain.

2️⃣
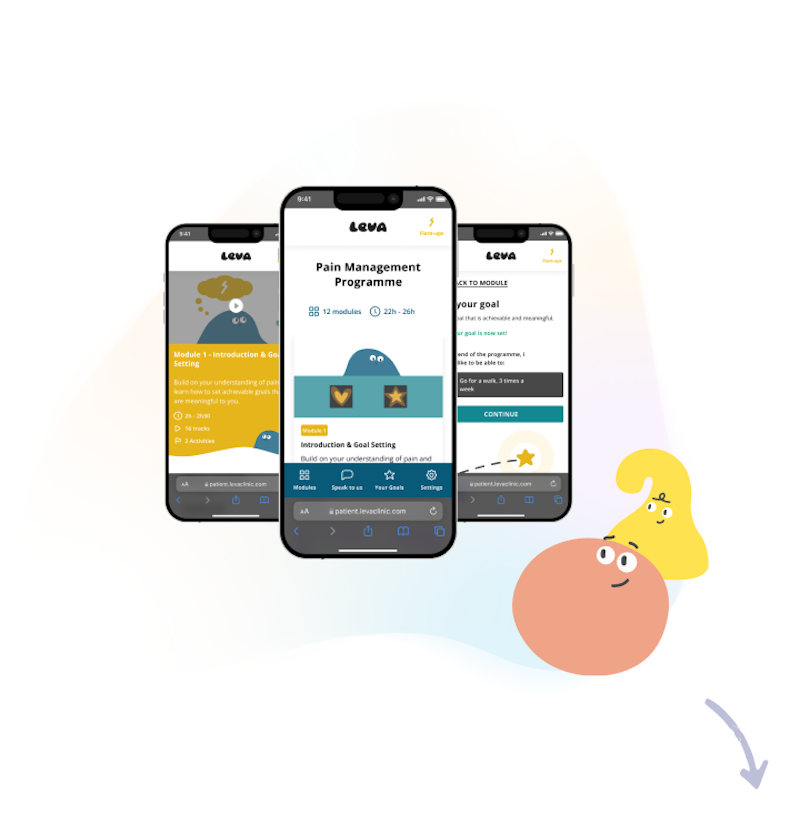
Tools to apply pain science for lasting change
Unlock the latest pain science (without the ‘painsplaining’)
Prepare to dive deeper into the intricate world of pain. We won't just throw jargon at you, we'll guide you through the latest scientific insights in a way that not only makes sense but empowers you to take meaningful action. Think of it as brain-training for your pain journey
3️⃣
Cannabis-based medication to replace traditional painkillers
It can be an effective and safe form of pain relief
Our data of patients on cannabis-based medicine plans shows 94% of patients report pain severity improvement, 59% stopped opioid usage and a 50% reduction in depression and anxiety †
Since 2018 it’s been legal for specialist medical consultants to prescribe.


Results
Data analysed by Imperial College London and Drug Science concluded...
50% reduction in anxiety and depression †
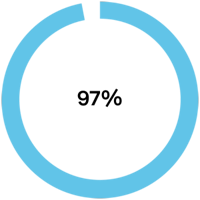
97% of patients reported no side effects †
94% of patients reported pain severity improvement †

59% stopped opioid usage †
Why Leva?
Hundreds have entrusted us with their care already. See how we compare against alternative options.
vs. NHS pain clinics
Skip the wait
We're big fans of the NHS (our clinical team all work within it). With huge demand, it can take up to 2 years to see someone who knows about your pain, and you might not get much time with them. With Leva, you can see someone in as little as 10 days. Plus, access cannabis-based medicine to help.
vs. going private
Why pay for generic advice?
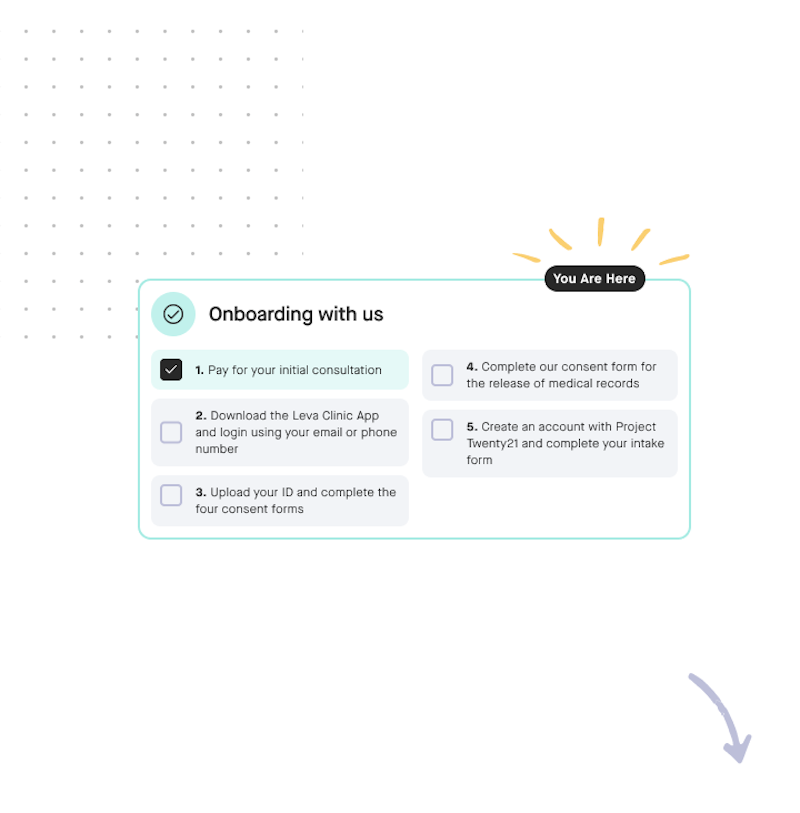
Paying for private appointments can be punishingly expensive, especially if pain impacts your finances. Why pay for generic advice? We’ve packed it into our app so you only pay a consultant’s time to help make it work for you.
vs. medical cannabis clinics
More than medication
We’re specialists in pain who prescribe medical cannabis, not the other way around. Our 3-in-1 approach tackles the root of your pain to help you find days when you don’t feel the need for any medication - including cannabis-based - but know it’s there if you need it. For the sake of your health, confidence and finances
A typical first 3 month programme

Sarah wants to take back control of her pain
She wants to live without fear of flare-ups and have her pain interfere less in her daily life and sleep.
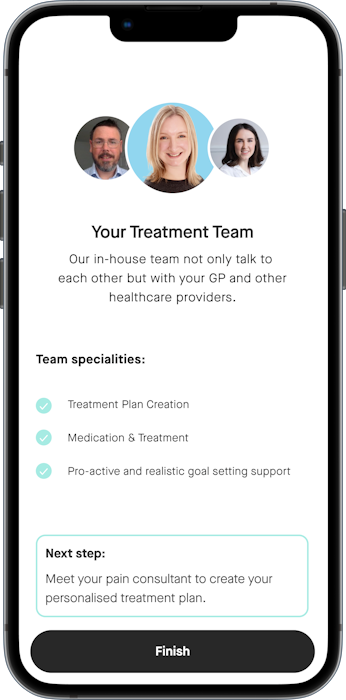
Sarah decides to try Leva
She completes our short form to help us understand the impact of her pain. She has some questions about what to expect so books time to chat with us to answer them.
We believe we'll be able to help her and she believes we're a good fit.
Sarah books an initial pain assessment for 10 days from now and pays for the 3-month programme.
We match her with Dr Charlotte Small - a Consultant in Pain Medicine who has significant experience working with people living with conditions such as hers.

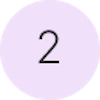
Sarah registers as a new patient
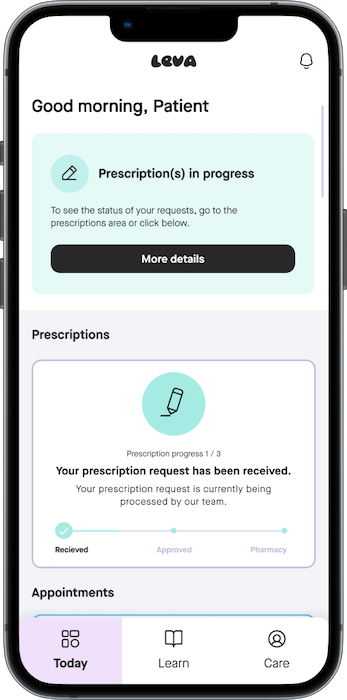
She downloads the user-friendly Leva Clinic app and follows the onboarding steps to prepare for her first consultation.
She requests a 'Summary Care Record' from her GP and the Leva team are able to assist her obtaining it.
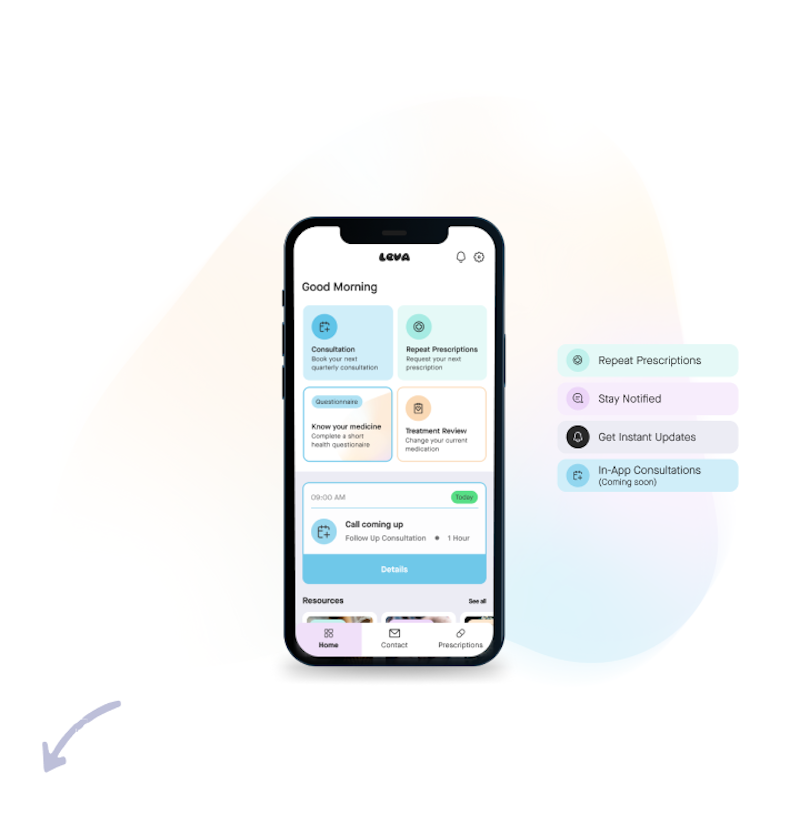

Sarah sees her consultant for the first time
Day 1 of care
Sarah has her first meeting with Dr. Small. During this meeting, Dr. Small talks about her treatment goals and discusses her medical history.
Dr. Small takes the time to understand how pain affects her life and what she'd like to achieve. They work together to understand what hasn't been effective in her previous treatments.
All of Sarah's options are discussed with her, including an introduction to cannabis-based medication. Dr. Small assesses all of Sarah's existing medication.
Together they create a plan that goes beyond medication to help Sarah achieve her goal of less pain interference with daily life and sleep.
They agree to begin to safely reduce some of the opioid medication Sarah was prescribed. Cannabis-based medication is introduced to help relieve pain.
Dr. Small writes to Sarah's GP to keep them informed about the treatment changes.

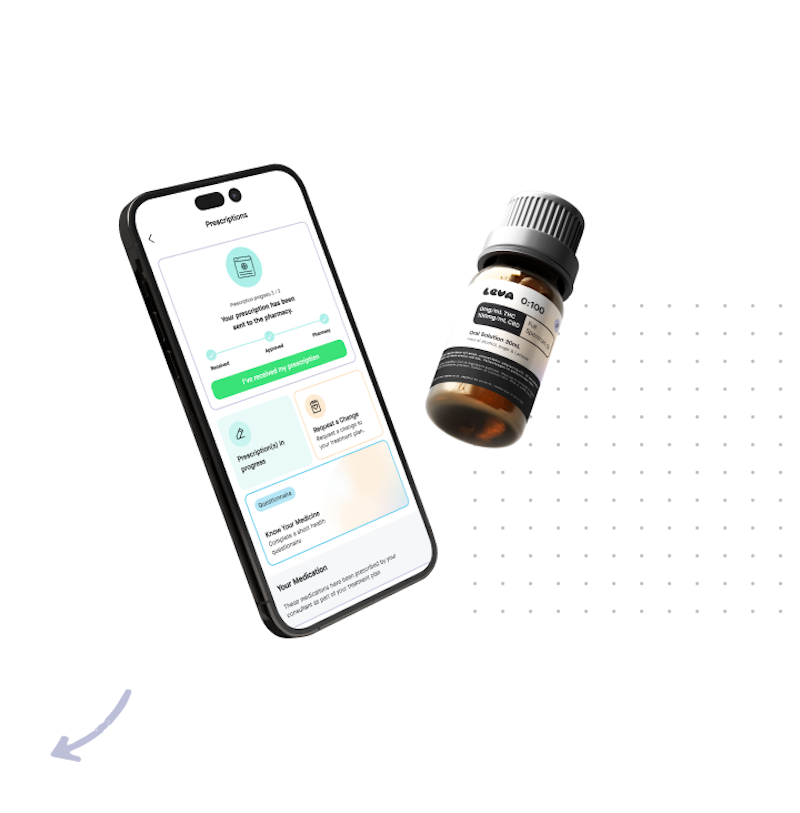
Sarah receives her prescription
Shortly after the consultation
After a second opinion from another consultant, Sarah receives a notification in the app that her prescription has been sent to the pharmacy.
The pharmacy contact her to gather details and payment for the medication. The prescription costs £130 for a 4-6 week supply and they arrange the delivery of discreetly to her home.

Sarah begins her new treatment plan
Within a week
Sarah receives her medication and begins her treatment plan. She has some questions before she first tries her new medication and our clinical support team happily help answer her questions.
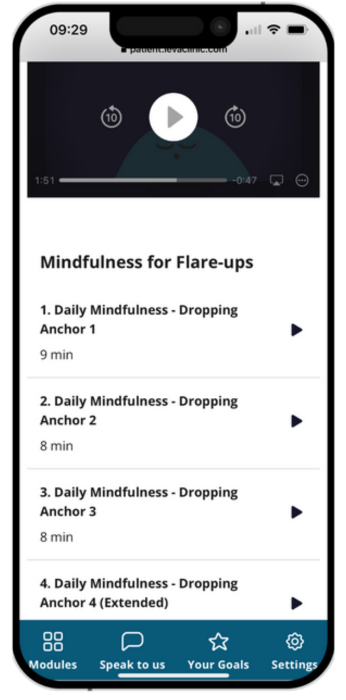
Sarah starts the online digital pain management programme. The 'bus' metaphor helps her understand her pain in a new way and she finds the pain-specific mindfulness practices helpful.
She RSVPs for an upcoming event led by consultant physiotherapist Diarmuid to dive deeper into the topics raised and ask questions she has. Others living with pain will be at the event too.

Sarah has a follow-up halfway through
After 6 weeks
Sarah books into a complimentary follow-up with Angie - a pain nurse specialist who works under Dr. Small.
Angie checks how Sarah is doing and makes slight adjustments to her treatment plan. Angie explains that this process often involves trying different things to see what works best. Angie also answers some new questions Sarah has about her medication and reassures her about a new physical sensation Sarah has experienced.

Sarah decides to continue for another 3 months
After 3 months
The new treatment plan has helped Sarah to start to find pain-life balance.
Sarah has started to have quality sleep and is beginning to find pain interfering less with her daily life. She doesn't experience negative side effects from the new medication and it effectively keeps her pain flare-ups at bay.
She decides to continue using the medication and begins another 3 month programme.
She appreciates the fact that she can consult with pain experts if she needs to adjust her prescription. She also enjoys the opportunity to attend live events about managing pain.




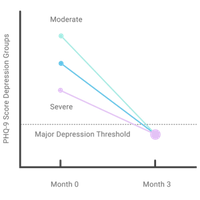
†
Data from proprietary sources, including collaboration with researchers from Imperial College and participation in research with Drug Science, indicate significant findings. BP (Pain Severity): 94% of patients reported an improvement in the severity of their pain. The percentage of chronic pain patients who reported any use of opioids decreased from 441 (55.1%) to 177 (22.1%), showing that over half (59.9%) of those previously using opioids had completely stopped. Additionally, more than 50% of patients with indications of major depression at initial assessment showed significant improvement after three months of treatment with medical cannabis and an online pain management program.